I believe many of you may have heard the term “โทรเวชกรรม” (Telemedicine) before. If you’re not familiar with it, this term may sound strange to you. However, since the outbreak of COVID-19, it has become a term that we have been hearing quite frequently. Telemedicine is a vital tool that connects patients and medical personnel, especially when meeting face-to-face is not possible.
Nevertheless, the Telemedicine system in Thailand has been continuously developed to meet the demands of different problems and situations. It also facilitates easier access to medical attention when one is ill or experiencing a health problem.
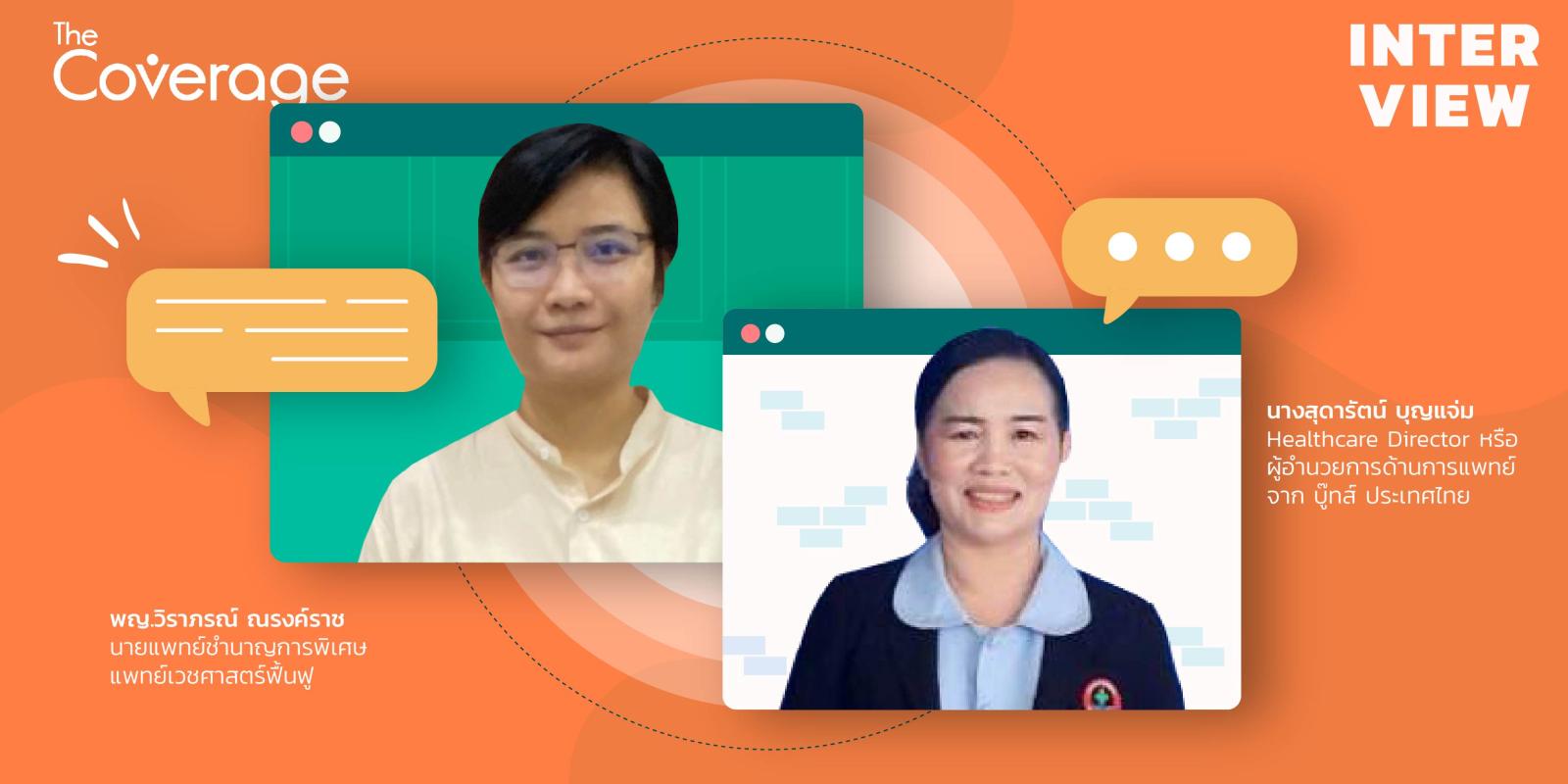
“The Coverage” had the privilege of interviewing Dr. Wiraporn Narongratch, a specialist in medical rehabilitation, and Ms. Sudarat Boonjaem, a health insurance officer and head of the collection department at Roi Et Hospital, about the use of Telemedicine at their hospital. The system they developed connects to community hospitals, making it possible for patients to receive medical services close to their homes. The system also links to the National Health Security Office’s payment system (NHSSO).
Dr. Wiraporn explained that the origin of the use of Telemedicine was due to the impact of COVID-19. Patients and their relatives were not able to keep their appointments, and physical therapy sessions had to rely on professionals who had to travel to the patients’ homes. To replace the follow-up sessions that used to occur at the hospital, the medical staff used applications such as Line or video calls to consult with patients while they were at home.
Overall, Telemedicine has proven to be a useful tool in facilitating access to medical care, especially during the pandemic. Its development in Thailand continues to evolve and improve to meet the demands of patients and health professionals.
Dr. Wiraporn explained that due to the limited number of medical rehabilitation doctors at Roi Et Hospital, there was only one doctor available (before adding two more doctors four months ago) and only one rehabilitation therapist with a specific medical background. This limitation made the implementation of Telemedicine not only for Roi Et Hospital but also for community hospitals that rely on physical therapists in each district.
With the service, patients who previously had to wait for rehabilitation, swallowing or communication training at Roi Et Hospital can now receive these services via the Telemedicine system developed by Dietz.asia and the attending doctor. Physical therapists in each neighboring community hospital who have completed training are also available to provide rehabilitation services to patients while receiving treatment.
“Telemedicine should help patients access services more easily, reduce travel to Roi Et Hospital, reduce waiting times for rehabilitation at the hospital, and be able to see medical rehabilitation doctors and specialists by simply requesting Telemedicine near their homes,” said Dr. Wiraporn
Community hospitals are the foundation of patient care. Regarding services at community hospitals, if patients have problems with swallowing, communication, etc., they will be scheduled for Telemedicine services. After confirming the appointment, the attending doctor will ask about their symptoms and assess them, and then rehabilitation will be conducted by a physical therapist via the system, with the participation of the attending physician.
Dr. Wiraporn stated that although the use of Dietz’s Telemedicine system is more reliable than the previous tools used, there are still limitations in the rehabilitation medicine field. Currently, Tele-Rehabilitation requires patients to make appointments with physical therapists as most rehabilitation patients are elderly or disabled and cannot access the system on their own.
Rehabilitation requires community hospital physical therapists nearby, so accessing the data system requires logging in through physical therapists, and personal patient data still needs to be entered into the hospital’s Hos xp system.
However, the result was that patients could receive treatment more frequently, once a month, rather than waiting for the doctor’s appointment every 3 months. Moreover, patients also appreciate the convenience of treatment because they can talk in real-time, which allows them to ask and answer questions. However, for physical evaluations, it is still essential to examine the patient in person. Nevertheless, it is better than patients feeling overwhelmed by traveling and waiting, which leads to them disappearing from the treatment system.
Before providing services, there must be a table talk to make it easier to “claim”
Ms. Sudarat explains that Roi Et Hospital is another service provider that participated in the long-distance health service project in July of last year, with the aim of reducing congestion. However, when the COVID-19 situation arose, it was assessed that the long-distance system was beneficial to the service recipients. Therefore, they joined, and rehabilitation medicine was one of the diseases sent.
At the same time, before starting the service, there would be a meeting between the health insurance group, doctors, and related personnel to discuss what information each group of patients needs to input into the Hos xp system, allowing the insurance group to check and claim easily. It is certain that claiming is not difficult if there is clear communication.
Ms. Sudarat stated that she had personally been a lecturer to share information about various funds of the NHSO to the community hospital so that they could be informed about service systems or service claim issues. Regarding the Telemedicine service claim of Roi Et Hospital, software has also been developed to connect the E-Claim system of the NHSO and the Hos xp of the hospital for service payment reimbursement.
As for the reason why there must be a connection, it is because claiming is not only for Telemedicine services, as there are other funds connected to the NHSO. This is like a sieve that needs to be sorted to see which parts can be claimed from the NHSO and which cannot.
Ms. Sudarat expands the reach of Roi Et Hospital’s service in caring for stroke patients by providing long-distance consultation and providing knowledge and understanding about the disease to patients and their families. This allows the hospital to provide more effective care and helps prevent recurrence.
 Eng
Eng
 ไทย
ไทย  seolounge
seolounge